A comprehensive dilated eye exam by an ophthalmologist can detect a multitude of systemic diseases and is often the first indication of many disease processes. The retinal blood vessels are the only place where a doctor can directly view your circulation without the need for expensive invasive tests like angiograms, CT scans, or MRI. The eyes are truly the window through which we view the rest of the body.
What can my ophthalmologist diagnose from a dilated eye exam?
DIABETES
It is recommended that all diabetics have a dilated eye exam at least once a year. Pregnant women with gestational diabetes may require an exam every trimester.
Diabetes can cause transient blurry vision when first diagnosed due to swelling of your natural lens. This is often one of the first signs of elevated blood sugar. It can also cause a specific type of diabetic cataract causing significant glare and difficulty reading. Diabetes can even cause age related cataracts to progress at a faster pace. Diabetics are also at greater risk of developing glaucoma.
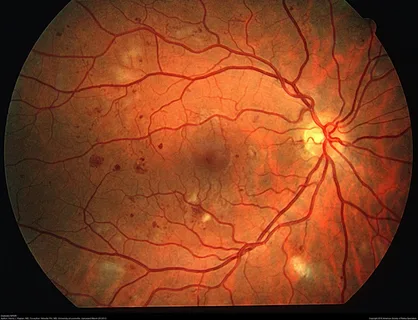
A more serious complication of diabetes affects the back of the eye and can lead to severe visual loss from swelling in the retina. Leakage of fluid or blood from the retinal vessels can progress, leading to hemorrhages and even retinal detachment. What your doctor sees in the retina closely mimics the appearance and function of the vessels in your kidneys and feet.
HYPERTENSION
High blood pressure also causes damage to the retinal vessels. Mild to moderate hypertension is characterized by changes in the vessels that are similar to those seen in early diabetic retinopathy. More acute rises in blood pressure can cause swelling of the optic nerve and a sudden change in vision in one or both eyes.
STROKES
There are several strokes that can directly affect vision. Blood flow through any of the vessels that supply the eye can be disrupted by blood clots, inflammation, or vasospasm. Risk factors for retinal artery or vein occlusions include older age, smoking, high blood pressure, diabetes, obesity, cardiovascular disease and clotting disorders, including malignancy.
Stokes can also affect any of the six muscles that move the eyes up, down, left and right, causing a sudden onset of double vision.
Stokes affecting any part of the visual pathway from the optic nerve to the visual processing centers in the brain can cause a sudden painless loss of vision in one or both eyes. This may affect the entire field of vision or just part of the vision in one or both eyes.
AUTOIMMUNE DISEASES
Many autoimmune diseases like rheumatoid arthritis, lupus, polymyalgia rheumatica and colitis are diagnosed because of ocular manifestations. Iritis, or uveitis, is an inflammatory condition that can affect all layers of the eye. Symptoms may include pain, redness, light sensitivity, decrease in vision and floaters. Some people may be entirely asymptomatic. Treatment includes treating the inflammation and pressure in the eye along with systemic medications prescribed by a primary care doctor or rheumatologist to treat the underlying condition. Complications of these conditions can also lead to glaucoma and cataract formation.
INFECTIONS
Bacterial, viral, fungal and parasitic infections can cause inflammation inside the eye that can mimic auto-immune uveitis. Tuberculosis, Lyme disease, CMV (mono), Herpes Zoster (Shingles) Herpes Simplex, Syphilis, Toxoplasmosis, Histoplasmosis, HIV and several others can cause ocular inflammation with subsequent loss of vision
CANCERS
Several cancers such as breast, lung and prostate cancer tend to metastasize to the eye. Many are detected on routine eye exams before symptoms occur. Primary ocular tumors such as melanoma can be detected by a dilated eye exam. Basal cell, squamous cell and other pre-cancerous lesions have a predilection for the eyelids. Leukemias and lymphomas often present with ocular findings.
MEDICATIONS
Numerous systemic medications cause damage to the eyes and may require baseline screening and regularly scheduled eye exams with ancillary testing to detect signs of toxicity. Plaquenil (hydroxychloroquine) used for rheumatologic diseases, can cause damage to the macula. Yearly dilated exams and visual field testing are needed to screen for irreversible visual loss. Amiodarone (atrial fibrillation) and Ethambutol (TB/MAC) can cause damage to the optic nerve and require regular monitoring by an ophthalmologist. Topamax used for migraines and weight loss, can cause a sudden onset of angle closure glaucoma. Even common medications such as doxycycline, sulfa and hormone replacements can cause a condition that mimics signs of a brain tumor causing headaches, dimming of vision and visual field loss.